What’s the Difference Between ASD and ADHD?
April 28, 2022
April 28, 2022

ASD and ADHD: These two acronyms have some of the same letters, some of the same types of challenges, and can appear in the same individuals, but the conditions have more differences than you might guess.

If you’re here on our site, chances are, you have some tie to autism spectrum disorder (ASD). The signs of autism may already be familiar to you, but they can be confused with the symptoms of attention deficit hyperactivity disorder (ADHD). In many cases, they can present alongside of each other.
Since the co-occurrence of autism and ADHD is high – research shows some rates as high as 50%** – we connected with Hopebridge clinical psychologist, Amaurita Kanai, PsyD, HSPP, to give parents more insight around the similarities and differences. Not only does Dr. Kanai have experience in both diagnoses, including conducting testing for autism at Hopebridge, but she has two sons who are both diagnosed with ASD and ADHD.
Here is what she wants to share with other families about autism and ADHD:
I understand what families are going through when trying to navigate autism and ADHD. Now ages 8 years and 15 years, I went through the process with my own kids. One is currently in full-time applied behavior analysis (ABA therapy) at Hopebridge, and the other attends a charter school for high school. But I was once right where you are.
Like autism spectrum disorder, attention deficit hyperactivity disorder falls in the category of neurodevelopmental conditions. Most of the symptoms of ADHD start to affect a child once they are of school age. There are three major ways ADHD can present:
Some of these behaviors overlap with those of autism, whereas others may seem quite the opposite. So how is a parent or physician supposed to know what these symptoms mean?
Though our evaluations at Hopebridge are focused on autism, the topic of ADHD can arise, so I like to ask parents, “how long has this been going on?”
This is because autism is a lifelong condition, yet ADHD is more of an emerging condition. The differences between the two can be seen in how the child responds to the demands being put on them.
The impairments related to autism start at a young age, even as early as infancy or toddlerhood. These can appear as differences in socialization, rigidity, routine preferences, focusing for long periods of time and a preference to play alone. In turn, demands also start young; you want the child to be able to look at you, smile at you and play with you.
ADHD starts to impact children around school age. Kids with autism are typically drawn to routine, but kids with ADHD tend to have a difficult time with routines, memorizing and organizing. Just as a child with autism might line up toys, a kid with ADHD might throw them everywhere. Kids also won’t get those demands to organize their backpack full of homework or listen to instructions until they are old enough to go to school, which is why we often do not notice the symptoms emerge until they are older.
Here are some of the ways ASD and ADHD overlap:
Even though we don’t want parents to diagnose on their own, we do want to give caregivers some direction. When determining where your child might need more support, try to focus on the underlying function of each area. For instance, is it a social deficit or are they not able to focus and pay attention? Does the child have the skillset but is just not able to focus long enough to use it, or does the child not have that innate skillset at all? If the latter is the case, then we are likely looking more towards autism.
While some parents might question whether their child has autism or ADHD, in many cases, they may have both. As research continues to grow around each condition, so has our understanding in how they impact each other. There is still a gap in the literature as to why these two conditions are often co-occurring, but it does show that if an individual has one set of symptoms, they have a higher chance of experiencing the other set of symptoms, as well.

When we have a child with both, we often see more of the internalizing symptoms of ASD, like isolation, fixation on interests and communication challenges. In this same child, we might see the externalizing features of ADHD, like jumping between activities, body movements that are not necessarily organized, fidgeting, and difficulty with attention and focus. There may be a few symptoms of each that impact the individual’s ability to function, but each child is different.
Here’s a “real world” example for you, too. My oldest son recently went back to school after a break from school due to the Covid-19. He was really excited to get back into the swing of things and focus on tornadoes – he’s always loved things that spin – but he completely forgot to wear a coat! He was so focused on what he wanted to do that he forgot to put it on before he left.
The profile of how symptoms appear is going to be different for each individual.
With ADHD, the frontline treatment usually consists of a prescriber on the team, so parents might look into medication, in addition to behavioral therapy. With autism, the frontline is behavioral interventions, such as ABA therapy. When a child has both, parents likely want to look into all of these angles for treatment.

To determine the proper course for treatment, behavior plans should look at how the conditions impact the ability of the child’s engagement in treatment. Understanding how these diagnoses would impact a child’s ability to progress in treatment is essential.
For instance, therapists need to understand if the child has the ability to focus and is avoiding or escaping, or if they do not have the ability in the first place, as focus may be impaired if they have ADHD. When there is a diagnosis, the therapy team can better understand and conceptualize a child and provide them with the correct care and motivation. Otherwise, they might be demanding too much from a child who is not able to give their attention.
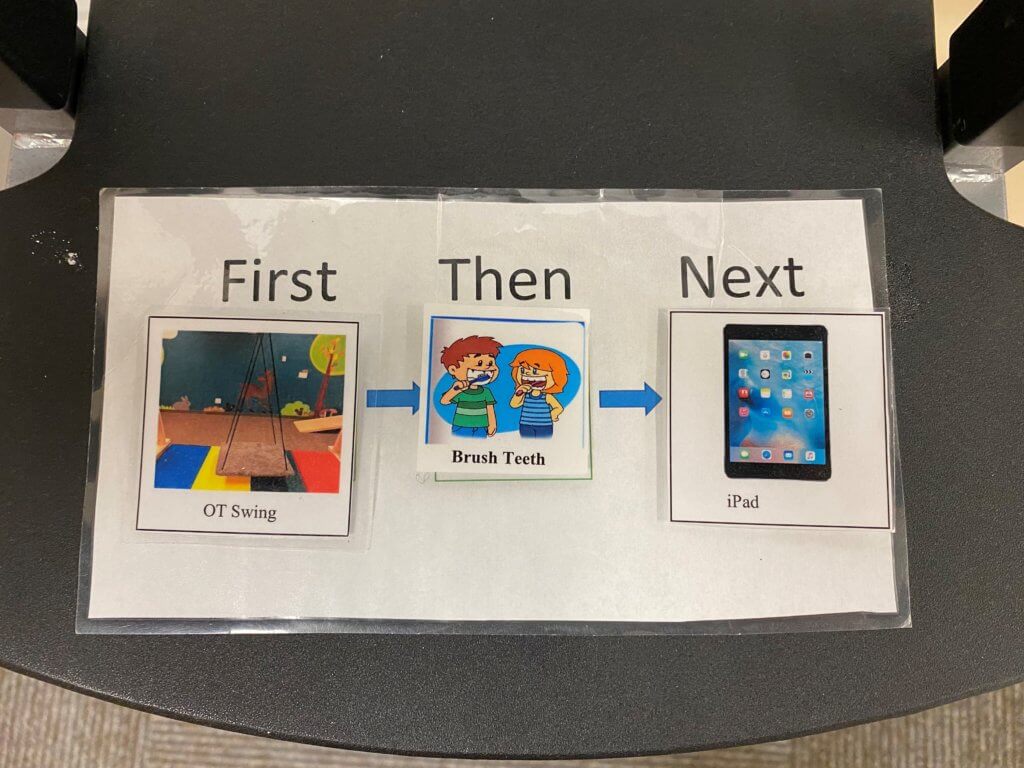
Reinforcers might need to be different for a child who has co-occurring ADHD, rather than a child who just has the symptoms of autism. Therapists might need to add a little more movement or sensory games into the session, and possibly jump from activity to activity more often.
The treatment team should be able to adjust, because if they know both diagnoses are present, they can approach them from different areas—one from the medication side, one from the behavioral side, for instance. Occupational therapy and speech therapy might also be indicated for a child with both diagnoses.
The first step in finding out whether your child has ASD or ADHD – or both – is to get in touch with your child’s primary care physician. Make notes ahead of time and review your concerns with the physician. If your child is already in school, ask their teacher about it to add to your own notes.

Note whether you have concerns around your child’s self-esteem. Are they feeling a little blue or having a tough time with social skills even though you know they want to make those connections? Or, maybe you opened their desk during a parent-teacher night at school and were surprised to find it a mess with papers and supplies everywhere. Make note of everything to share with the physician.
The pediatrician can perform an initial screening for ASD and ADHD, but your next step is to get referrals for specialists. Child clinical psychologists, neurologists and developmental pediatricians can help you clarify your concerns. Psychiatrists can also be useful when you’re looking to discuss medication. Get as many treatment team members who are familiar with developmental delays and disorders as possible.
Getting a bigger picture of the child is always encouraged. Psychological testing, like that of testing for autism, is something I recommend to help you do this. We do that right here at Hopebridge if you are looking for an evaluation to find out whether your child has autism.
Advocate for your child. I understand that parents may sometimes feel as though they are not being heard by physicians. I noticed my oldest son’s rocking, hand-flapping and speech delay all from a young age, which allowed me to get him support, but my youngest son was diagnosed late, even though I am a clinical psychologist. His symptoms of autism emerged later and some of the physicians were not as receptive to my understanding of my own child as I would have hoped. If your child hasn’t followed a typical course, keep asking questions until you get to the right person. This doesn’t mean there will always be a diagnosis, but you do need to be heard.
My oldest son was diagnosed with autism much earlier and therefore had access to interventions earlier, and I can see the difference. If you feel like there’s something going on with your child, don’t give up until you have the answers and intervention that you need and your child deserves.
I am here to give parents hope. My kids are doing well and yours can, too.
– Amaurita Kanai, PhD, HSPP and mother of two
Does this piece have you wondering, “Is it autism?” We want to help your family get the answers you need. Reach out to us to arrange autism testing, ABA therapy or other interdisciplinary services at one of our locations around the country.
References:
**Rong Y, Yang C-J, Jin Y, Wang Y. Prevalence of attention-deficit/hyperactivity disorder in individuals with autism spectrum disorder: a meta-analysis. Res Autism Spectr Disord. (2021) 83:101759. doi: 10.1016/j.rasd.2021.101759 https://www.sciencedirect.com/science/article/abs/pii/S1750946721000349?via%3Dihub
*Informed consent was obtained from the participants in this article. This information should not be captured and reused without express permission from Hopebridge, LLC.
Parenting Resources
October 22, 2021
Tips for Adjusting to the Time Change for Autism Families
Parenting Resources
February 10, 2022
Valentine’s Day Communication Tools and Sensory Activities for Kids with Autism
Hopebridge in the News
March 26, 2019
Hopebridge expands into Macon with state-of-the-art autism therapy center